Healthcare Informatics – Characteristics of Respondents
Of the 101 respondents to the Healthcare Informatics Survey, the majority were older than 40 years (54.5%), male (62.0%), and white (70.1%) (Table 1). Respondents may identify more than one role. Most were physicians (44.6%), followed by data scientists (36.6%). Most of the respondents reported that they have been practicing informatics for more than 10 years (54.5%).
Most felt they were very well informed (41.6%) or fairly informed (48.5%) about AI/ML, with the majority reporting that they had taken coursework on the topic (61.4% ) or doing research on this topic (68.3%). A large portion also reported that they have worked on deploying AI/ML (42.6%).
Clinician survey – characteristics of respondents
Of the 607 US-based respondents to the Clinician Survey, the majority were 40 years of age or younger (69.9%), female (55.7%), and white (68.2%) (Table 2). Physicians constituted 70.7% of the respondents, of whom 45.4% were trained. Hospital medicine was the most common specialty (52.1%) followed by hematology (20.8%). The majority of respondents (65.8%) reported deciding whether a patient needed VTE prophylaxis every day. Only 20.5% of respondents reported that they have used AI/ML to inform their clinical practice. The majority did not (57.9%) or were unsure (21.6%).
Healthcare Informatics – Experiments with AI/ML
Most informatics (62.6%) reported that their organization was using or developing AI/ML for healthcare. Of these 62 respondents, the majority described the status of AI/ML in their organization as having at least one model in use (82.3%), and that their organizations primarily develop models themselves ( 81.4%). Less than half (45.8%) reported using third-party vendors or partnering with local universities (28.8%).
Respondents who reported developing AI/ML systems used Python (76.6%), R (45.3%), and toolkits (42.2%). Among respondents who stated which toolkit they preferred, the most commonly cited were Scikit-learn and TensorFlow.
Healthcare Informatics – Approaches to AI/ML
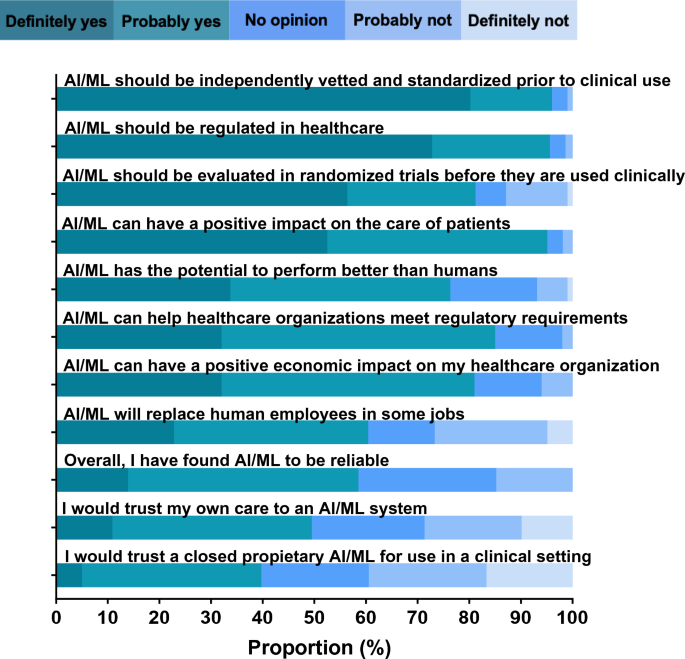
Majority of informants agreed that AI/ML can positively impact patient care (95.0%), help healthcare organizations meet regulatory requirements (95.0%) is, and can have a positive economic impact on their health care organization (81.0%). ) (Fig. 1, Supplementary Table 1). Informatics experts mostly agreed that AI/ML has the potential to outperform humans (76.3%) and will replace human employees in some jobs (60.4%). Respondents found AI/ML to be reliable overall (58.5%) and would trust their care to an AI/ML system (49.5%). However, less than half would trust a closed proprietary system (39.7%). Most informatics experts agreed that AI/ML should be independently evaluated and standardized before being used in clinical settings (96.0%), regulated (95.6%), and randomized controlled trials (81.2%).
Informant attitudes toward AI/ML (n = 101).
The three most common reasons respondents identified as barriers to the successful development of AI/ML in healthcare were data quality (67.3%), lack of standardization (39.8%), and healthcare Difficulties of acceptance by providers were (35.7%).
Healthcare Informatics – Attitudes towards AI/ML for blood coagulation management
The majority of informants agreed that AI/ML can be used for clinical management of blood clots (56.0% 95% CI 46–66%). Most of these 56 respondents agreed that AI/ML should be used for risk stratification (94.6%), radiologic accuracy (87.5%), surveillance (80.4%), diagnosis (73.2%), and treatment ( 73.2%) (Fig. 1) can be used for 2). Four respondents suggested potential additional uses for AI/ML: monitoring of clot dissolution, warfarin dosing, shared decision making, and treatment during acute versus chronic recovery phases. All respondents were asked about perceived barriers, and the most commonly cited barriers were lack of transparency with AI/ML systems (48.5%), concerns that clinicians are not using AI/ML systems will (34.7%), and concerns about responsibility (24.8%) (Supplementary Table 2). Informaticians who identified as clinicians were more likely to believe that AI could help with VTE than those who did not identify as clinicians, although this difference was not statistically significant. was not (66.7% vs. 47.3%, respectively; p = 0.052). Respondents from organizations that had implemented AI were less likely to think that AI could help with VTE than organizations that had not implemented AI (59.0% vs. 48.7%; p = 0.32).
Potential applications of AI/ML for the management of blood coagulation (n = 56).
All respondents were asked the free-text question, “What else should be considered when using AI/ML to aid in the clinical management of blood clots?” There were 37 responses, six of which were removed from the analysis because they did not answer the questions. Of the remaining 31 responses, almost all were related to system validation and discussed factors related to scrutiny, bias and transparency. A number of responses discussed deployment, and a few responses touched on the importance of clinician supervision (themes in Table 3 ; coding tree in Supplementary Table 3 ).